I’m not in much mood to write a post today. And I suppose I could just not write anything. Nobody has a paid subscription guaranteeing a publishable post. I’m on no program mandating so many words written per week. But because I’m a trooper (and. It just another pretty face), you’re getting a post whether you want one or not.
There has been so much going on since last Monday (and I’m not even considering what Dingy Donny, J(ust) D(umb), and the South African American immigrant were up to) . I already told you the biggest news, the loss of little Jingle. When Jingle first went to live with the daughter he was more than a handful. It wasn’t too terribly long before he was acting only like a little terror and a few more months until he because a reasonably well-behaved canine gentleman. He will be missed.
Thing Two also was brought up in Thursday’s post. That was an already planned procedure that took way too long. It was a simple enough thing. A little quickly rerouting of a vein in my arm. We got to the hooray at 9am and left at 5:15 that afternoon for a roughly hour long procedure. To facilitate the actual surgery I was given a nerve block which rendered my arm absolutely useless for 2 days. Not just numb, but dead weight hanging off my shoulder. I had to carry my arm around in a sling or I’d leave it behind.
Item the third has been this headache I’ve been carrying around for the last 4 days. I used to be subject to terrible vascular headaches. Nothing helped. Somewhere along the way, while is was researching something at the hospital, I came across an old article (older than me even) that described very low doses of an old, old antidepressant (which was probably newfangled when the article was written) to treat headaches. I convinced my PCP it made sense to try it and if it didn’t make sense to her I knew a lot of other doctors I could go to. (These were really annoying headaches and I was not above threatening taking my medical business elsewhere.) Well…to make a long story short (I know, too late), the pills worked. Until Thursday.
And finally, I really want some ice cream.
There. Now you have your post, and in the process I actually feel a little better. It’s odd becuase there weren’t a lot of positive things mentioned and that’s a sure-fire way of feeling calmer and at peace. (Is that sure-fire or sure-fired?) Oddly enough, we wrote about feeling calm and at peace in last week’s Uplift. Take a look at Location, location, location.
While you’re there, consider joining the ROAMcare community and subscribe to have Uplift delivered to your email as soon as it hits the website. In addition to an Uplift release every Wednesday, you will also receive weekly our Monday Moment of Motivation and the email exclusive Flashback Friday repost of one of our most loved publications every Friday. All free and available now at ROAMcare.org.

 While the donor’s surgeons are finishing their procedure the recipient’s receiving location is prepared by a second surgical team. The recipient surgery is performed through an open incision and two attending transplant surgeons, in my case one of them also a urological surgeon, will operate. Unless there is a medically necessary reason, the recipient’s native kidneys are not removed. The donated kidney will be placed in an abdominal lower quadrant, usually the right although in my case because of previous surgeries and that space already occupied, it will be placed in the left lower quadrant. The renal vessels and ureter from the native kidneys are transpositioned and the recipient is closed up and sent off to recover.
While the donor’s surgeons are finishing their procedure the recipient’s receiving location is prepared by a second surgical team. The recipient surgery is performed through an open incision and two attending transplant surgeons, in my case one of them also a urological surgeon, will operate. Unless there is a medically necessary reason, the recipient’s native kidneys are not removed. The donated kidney will be placed in an abdominal lower quadrant, usually the right although in my case because of previous surgeries and that space already occupied, it will be placed in the left lower quadrant. The renal vessels and ureter from the native kidneys are transpositioned and the recipient is closed up and sent off to recover.
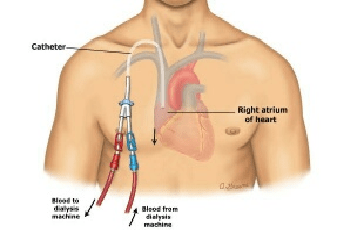 The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.
The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.