Last week I took a shot at regaling you with tales of spending a week in the hospital and coming home alone. Naturally the perfect followup to that would be (to take a shot at) regaling you with tales of spending that recovery week not quite alone. Yes, even though I made a big thing out of how hard it is to not be well and be alone, versus when you are a one of two, I wasn’t completely alone in my recovery week. Not quite not alone but definitely not alone.
I closed last week’s post with, “When one of two is missing, the void seems bigger than when one of one is gone. And when one of one returns, the welcome home is much less welcoming. I can probably write an entire post on that. Maybe I will someday.” Never to not pick up such a tempting gauntlet as that, I will accept my own challenge. Sort of.
First, to those who had asked, I am fine and anticipate I will grow even finer as the days march by. I made it through the first week out of the hospital without returning to the hospital and that’s not something I can say about all of my discharges. Fortunately, I had a lot of help. As I said, I was not completely alone last week. I had help. Not “one of two” help, maybe more like “one of one-plus.” Between my daughter and my sisters for some physical assistances and a handful of friends for mental, emotional, and at times even comical support, the week moved along faster than I figured it would.
It is a big boost when someone you typically connect with primarily through text messages makes time in her schedule to call at least once a day every day to check on how things are going. It is as big an aid to recovery as having someone stop in to do the heavy lifting portions of the never-ending household chores that one with a newly prescribed 5 pound lifting limit and prohibitions against bending and stretching cannot take on alone. Yes, it is not a secret that physical recovery does not happen, or happens very slowly, without mental and emotional recovery tagging along.
I recall that first discharge from so many years ago, the physical helpers were there but there was a distinct void where someone, some ones, or anyone who might call just to see how things were going could have been. What was most disheartening was that there should have been at least one someone, but the call that came rather than a message of support was of the “I didn’t sign up to be a nursemaid” type. And with it a rather rapid descent from the stratospheric one of two to the heartbreaking loneliness of a one of less than one.
Fortunately, over the years I discovered a handful of contenders willing to be part of my one of one-plus entourage. True, the other one of a one of one-plus won’t be there to help you into bed, or to wake you when your due for medication or a dressing change, or tell you, “Sit still! I’m perfectly capable of making us breakfast,” as I imagine the other one of one of two would, somehow it is easy to imagine they would if things might had been just a bit different. And a one of one-plus will always be there on the other end of a phone call or text message, or email, or even a card or letter when you least expect it, or at least when you least are thinking about it for a while and add to your emotional recovery.
The best one of one-pluses are those who take their role seriously, as seriously as a one of two partner would. Maybe even more. Let’s face it, a lot of one of two partnerships exist because of some compromise or even a little unspoken quid pro quo. Sometimes a lot of quid pro quo. A one of one-plus is more selfless and unconditional. There is nothing you are getting back for your love and concern except maybe someone’s love and concern. A friend of mine, a one of one-plus with me, said “Being one of one can be isolating. Being one of two is ideal. But being one of many makes a community. We all need each other and do better when we feel cared for and important to somebody.” I suppose if we put all my one of one-pluses together we can make a “one of many” community. (Now that might make for an interesting blog too. In fact, that sounds like just the thing we’d post at the ROAMcare blog, Uplift! Maybe you should make a note in your calendar to check that out this Wednesday.)
Speaking of Uplift! In the latest post we wondered, if “In case” added to your declaration is a positive account of caution and a potential response to a situation, is “just in case” just a poor excuse for a poor choice? Read it here to see what we had to say about that.
Hey, here’s an extra thought if you know someone who could use a hand and you’re feeling one-plus-like. Dinners that can be heated and eaten are great but think outside the oven. Rides to labs or tests are great stress relievers and don’t often run unpredictably late like a doctor appointment may. And back in the food arena, if your someone is a big breakfast eater, a prepared morning meal is just as appreciated, if not more than an evening meal. A French toast casserole, or stack of frozen waffles makes a nice change for someone who may be too unsteady in the morning even to work a bowl of microwave oatmeal. My best meal “gift” ever was a bag of frozen breakfast burritos my daughter worked up. A few minutes in the microwave and a cup of yogurt with fresh fruit and I had a breakfast that kept me well through lunch and the only thing I needed to work was a spoon.


 On Thursday January 13, I drove myself across town to one of 3 clinics administering the more precious than gold elixir. About an hour later I actually felt better. The fever was low-grade rather than raging, the shaking and chills were reduced to a mild tremor, the squeezing headache relented, and the sore throat, eyes, sinuses, nose, in short everything north of the neck stopped hurting. I figure in 2 days I’ll probably be breathing again. Ha!
On Thursday January 13, I drove myself across town to one of 3 clinics administering the more precious than gold elixir. About an hour later I actually felt better. The fever was low-grade rather than raging, the shaking and chills were reduced to a mild tremor, the squeezing headache relented, and the sore throat, eyes, sinuses, nose, in short everything north of the neck stopped hurting. I figure in 2 days I’ll probably be breathing again. Ha!
 You recall my rants regarding remote controls. Too many buttons, too little function! Back in the 70s (yes, I really am that old) nurse call bells were pretty much that. In fact, the first hospital I worked at kept actual bells to distribute to patients in the event of a power failure. Today’s call bell alert mechanisms control lights, television power channel and volume, bed position, sleeping alarms, and might actually summon assistance by way of a two-way radio communication with a disembodied voice from somewhere deep in the building. My particular remote control/Dick Tracy wrist radio gets a lot of abuse pulled across the room, dropped on the floor, and otherwise tortured. This is an absolute true story. All of them are but you are going to say “Oh come on now!” when you read this so just keep in mind, this is an absolute true story. Among other things, my call button controls the room light (button A), controls a reading lamp (button B), controls the TV (TV), and summons assistance (stick figure of some bald dude). I was ready to call it another unsuccessful day and pressed button B to turn the reading lamp off but instead the main room light came on. Checking that I was indeed pressing the right button I tried again and the main light went off. Then I pushed button A because why not and the TV came on. Pressing button A a second time yielded no results so I pressed the stick figure button to report my equipment malfunction but instead of lighting up indicating a call had been initiated, the TV went off and the reading lamp came on. At this point I was back to having the reading lamp on and everything else off. I figured I could fall asleep under those circumstances and left well enough alone. Eventually someone would be in to check my blood pressure and I would report the broken control then.
You recall my rants regarding remote controls. Too many buttons, too little function! Back in the 70s (yes, I really am that old) nurse call bells were pretty much that. In fact, the first hospital I worked at kept actual bells to distribute to patients in the event of a power failure. Today’s call bell alert mechanisms control lights, television power channel and volume, bed position, sleeping alarms, and might actually summon assistance by way of a two-way radio communication with a disembodied voice from somewhere deep in the building. My particular remote control/Dick Tracy wrist radio gets a lot of abuse pulled across the room, dropped on the floor, and otherwise tortured. This is an absolute true story. All of them are but you are going to say “Oh come on now!” when you read this so just keep in mind, this is an absolute true story. Among other things, my call button controls the room light (button A), controls a reading lamp (button B), controls the TV (TV), and summons assistance (stick figure of some bald dude). I was ready to call it another unsuccessful day and pressed button B to turn the reading lamp off but instead the main room light came on. Checking that I was indeed pressing the right button I tried again and the main light went off. Then I pushed button A because why not and the TV came on. Pressing button A a second time yielded no results so I pressed the stick figure button to report my equipment malfunction but instead of lighting up indicating a call had been initiated, the TV went off and the reading lamp came on. At this point I was back to having the reading lamp on and everything else off. I figured I could fall asleep under those circumstances and left well enough alone. Eventually someone would be in to check my blood pressure and I would report the broken control then. While the donor’s surgeons are finishing their procedure the recipient’s receiving location is prepared by a second surgical team. The recipient surgery is performed through an open incision and two attending transplant surgeons, in my case one of them also a urological surgeon, will operate. Unless there is a medically necessary reason, the recipient’s native kidneys are not removed. The donated kidney will be placed in an abdominal lower quadrant, usually the right although in my case because of previous surgeries and that space already occupied, it will be placed in the left lower quadrant. The renal vessels and ureter from the native kidneys are transpositioned and the recipient is closed up and sent off to recover.
While the donor’s surgeons are finishing their procedure the recipient’s receiving location is prepared by a second surgical team. The recipient surgery is performed through an open incision and two attending transplant surgeons, in my case one of them also a urological surgeon, will operate. Unless there is a medically necessary reason, the recipient’s native kidneys are not removed. The donated kidney will be placed in an abdominal lower quadrant, usually the right although in my case because of previous surgeries and that space already occupied, it will be placed in the left lower quadrant. The renal vessels and ureter from the native kidneys are transpositioned and the recipient is closed up and sent off to recover.
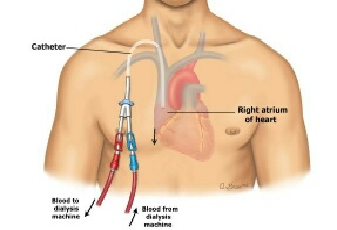 The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.
The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.