Because it is World Kidney Day, and only because it’s World Kidney Day, I’m going to talk about kidneys and then I’ll give you a few weeks without having to hear about my internal organs.
Since our last kidney transplant report I have lost one potential donor to high blood pressure. That leaves one who has now completed the evaluation and one with one test remaining and then of course the final review. That might bring up a couple questions for you. If it doesn’t, don’t worry, I’ll ask them. Does it seem to be taking a really long time and is it unusual to have a donor disqualified after such a long time into the process?
Honestly it is taking a bit longer than the average for these people to get through the evaluation process although not really by too much. I suppose if all the stars lined up and there was no waiting for appointments and if you had the most flexible schedule in the world and could be accommodating to the scheduling whims of a dozen different hospital departments you could breeze through the process in a couple months. But if you’re thinking the process is
…Step 1 hold sign up at hockey game looking for kidney,
…Step 2 sort through the 99,000 volunteers and pick the one with the best looking teeth,
…Step 3 meet in pre-op the following morning and plan to share a pitcher of beer later that day,
ummmm, no.
Under the best of circumstances it takes weeks and weeks because the process is a few more than 3 steps. And potential donors can be eliminated at any step, including the last.
The process pretty much follows the decreasing chance of elimination. That is, the step that would rule out most people as a donor is first, the second most common disqualifier then next, and so on.
A medical and family history is the first step along with a discussion of what is required for the evaluation, surgery, and recovery for a potential donor. At the same time, lab studies are drawn. Blood and tissue type compatibility is a must. If the donor candidate does not match the transplant candidate there are no further steps. In the spirit of the upcoming baseball season that means one strike and you’re out. There are no further reviews and no reconsiderations. If lab tests note suggestions of compromised renal function, unbalanced electrolytes, or heretofore unknown conditions such as diabetes, a committee will review the results and determine if the donor candidate can continue, be referred for treatment then reevaluated, or referred for treatment but disqualified.
Next are the cardiac and pulmonary functions. Will the donor’s heart and lungs get through the surgery and will they be strong enough to continue serving the donor well with the support of one remaining kidney? These steps include chest x-ray, EKG, stress test, and 24 hour blood pressure monitoring. At this point an abnormal return in one exam might require additional testing while the donor continues, additional testing while the donor holds, or disqualification. For example a slightly elevated blood pressure could require a second 24 hour test but the donor can proceed. A severely elevated blood pressure would hold the donor and refer him or her for new, modified, or additional treatment. A 24 hour blood pressure that remains within normal limits only with the use of more than one antihypertensive drug disqualifies the donor. In my particular set of donors there is one who was allowed to proceed pending a repeat 24 hour study ordered and then held and referred to cardiology for further review.
Next are renal function tests. You might think that if a person is considering donating a kidney the renal function tests would come sooner. People who know they have a renal impairment know not to begin the process. Nine out of 10 people with renal disease do not know it so why would this not be the first system reviewed? Many of these people know they have a family history or it will be suggested by the earlier lab studies so they may not ever reach this step. A donor who does not initially pass the renal function tests will be reviewed by the transplant committee. Here they will be held until a determination is made that the test will be repeated, the results were expected because of other physical characteristics of the candidate, or the donor is disqualified. In my set of donor candidates, one was held for a repeat evaluation then further reviewed and determined to be allowed to proceed.
Then comes the psychological review. Usually. In some cases when a donor candidate has a history that includes psychological, emotional, or mental medical concerns with or without medication management, the psychological review may come after the initial history and lab studies. Most often it is held here when the potential donor is only two steps from being or not being further referred to as a candidate. In its simplest term, this is when it gets real. A candidate will either move on or withdraw.
To this point each step contains multiple tests any of which can hold or disqualify a candidate. After each test the transplant committee reviews the results and determines the next step: proceed, proceed but reschedule and repeat, hold and repeat, hold and review, or withdraw.
The penultimate step is an abdominal CT Scan. This step is the last physical exam for the donor candidate. This step explores the candidate’s kidneys and their physical appearance and position and is used to confirm the kidneys are normal in size and shape, which is the preferred kidney for harvest, and that all surrounding organs and tissue appear normal and regular. Here a donor will be approved for final review, held for further study due to an inconclusive finding regarding either or both kidneys, held and referred to appropriate specialist for inclusive finding regarding surrounding organs, or disqualified. Among my donor candidate pool, one was referred to a specialist when a nearby organ appeared other than normal.
At the final step the donor’s results and findings are reviewed by the transplant committee who will recommend the candidate to donor status or recommend withdrawal. In the case of multiple donor candidates specific for a single transplant candidate, a recommendation of one or more with consideration to potential acceptance and viability of the donated organ may be made.
 So now that it took you so long to read about the process you may better understand why it is taking so long to complete the process. Each of my donor candidates was stopped at some point in the evaluation. One proceeded all the way to the CT Scan when a shadow was noted on a neighboring organ. The transplant committee interrupted the process and referred her to a specialist who in turn determined the shadow was not clinically significant and recommended her to continue which the transplant committed approved. One was held at the renal function test when the IV mediated glomerular filtration rate returned a slightly elevated result. The committee referred the result to one of its own nephrologists who recalculated the result and determined due to her physical structure it was within normal limits for her height, weight, and age and recommended to continue. One potential donor returned elevated 24 hour blood pressure results. She was allowed to move on to the renal function tests but had to reschedule a repeat 24 hour blood pressure monitor. The second 24 hour blood pressure results also returned elevated and she was referred to her cardiologist. Pending his review and finding, even though by this time she had passed the renal function tests, she was held from further candidate progress. Ultimately her blood pressure could be maintained within the standards expected for a kidney donor only with the use of two medications thus she was removed from the candidate pool.
So now that it took you so long to read about the process you may better understand why it is taking so long to complete the process. Each of my donor candidates was stopped at some point in the evaluation. One proceeded all the way to the CT Scan when a shadow was noted on a neighboring organ. The transplant committee interrupted the process and referred her to a specialist who in turn determined the shadow was not clinically significant and recommended her to continue which the transplant committed approved. One was held at the renal function test when the IV mediated glomerular filtration rate returned a slightly elevated result. The committee referred the result to one of its own nephrologists who recalculated the result and determined due to her physical structure it was within normal limits for her height, weight, and age and recommended to continue. One potential donor returned elevated 24 hour blood pressure results. She was allowed to move on to the renal function tests but had to reschedule a repeat 24 hour blood pressure monitor. The second 24 hour blood pressure results also returned elevated and she was referred to her cardiologist. Pending his review and finding, even though by this time she had passed the renal function tests, she was held from further candidate progress. Ultimately her blood pressure could be maintained within the standards expected for a kidney donor only with the use of two medications thus she was removed from the candidate pool.
So now with one candidate at final review and one awaiting an upcoming CT Scan, you might be reading one of the last installments in my search for a kidney. And if that’s the case it means you might soon get to start on a new journey, one of a new transplant recipient.
—–
Transplant Journey Posts
First Steps (Feb. 15, 2018)
The Next Step (March 15, 2018)
The Journey Continues (April 16, 2018)
More Steps (May 31, 2018)
Step 4: The List (July 12, 2018)
Step 1 Again…The Donor Perspective (Sept 6, 2018)
And The Wait Goes On (Oct. 18, 2018)
Caution: Rough Road Ahead (Nov. 19, 2018)
And The Wait Goes On (Jan. 24, 2019)
Other Related Posts
Walk This Way…or That (March 9, 2017)
Looking Good (May 18, 2017)
Technical Resistance (May 25, 2017)
Those Who Should Know Better (July 24, 2017)
Cramming for Finals (May 3, 2018)
Make Mine Rare. Or Not (Feb. 28. 2019)
 Some spare parts are less obvious and often invisible. Artificial lenses often reside in post cataract surgery eyes correcting clearer but weaker vision; pacemakers and implanted defibrillators keep weak hearts working stronger. A friend’s father was an early recipient of an early implanted defibrillator. It worked dandily, even way back then. Except whenever someone triggered the garage door opener they also triggered a mild shock to his heart. They fixed that by replacing the opener. Easier than replacing the father. And some spare parts are outright replacements like a swapped out heart, lung, pancreas, liver, even a kidney.
Some spare parts are less obvious and often invisible. Artificial lenses often reside in post cataract surgery eyes correcting clearer but weaker vision; pacemakers and implanted defibrillators keep weak hearts working stronger. A friend’s father was an early recipient of an early implanted defibrillator. It worked dandily, even way back then. Except whenever someone triggered the garage door opener they also triggered a mild shock to his heart. They fixed that by replacing the opener. Easier than replacing the father. And some spare parts are outright replacements like a swapped out heart, lung, pancreas, liver, even a kidney.
 So now that it took you so long to read about the process you may better understand why it is taking so long to complete the process. Each of my donor candidates was stopped at some point in the evaluation. One proceeded all the way to the CT Scan when a shadow was noted on a neighboring organ. The transplant committee interrupted the process and referred her to a specialist who in turn determined the shadow was not clinically significant and recommended her to continue which the transplant committed approved. One was held at the renal function test when the IV mediated glomerular filtration rate returned a slightly elevated result. The committee referred the result to one of its own nephrologists who recalculated the result and determined due to her physical structure it was within normal limits for her height, weight, and age and recommended to continue. One potential donor returned elevated 24 hour blood pressure results. She was allowed to move on to the renal function tests but had to reschedule a repeat 24 hour blood pressure monitor. The second 24 hour blood pressure results also returned elevated and she was referred to her cardiologist. Pending his review and finding, even though by this time she had passed the renal function tests, she was held from further candidate progress. Ultimately her blood pressure could be maintained within the standards expected for a kidney donor only with the use of two medications thus she was removed from the candidate pool.
So now that it took you so long to read about the process you may better understand why it is taking so long to complete the process. Each of my donor candidates was stopped at some point in the evaluation. One proceeded all the way to the CT Scan when a shadow was noted on a neighboring organ. The transplant committee interrupted the process and referred her to a specialist who in turn determined the shadow was not clinically significant and recommended her to continue which the transplant committed approved. One was held at the renal function test when the IV mediated glomerular filtration rate returned a slightly elevated result. The committee referred the result to one of its own nephrologists who recalculated the result and determined due to her physical structure it was within normal limits for her height, weight, and age and recommended to continue. One potential donor returned elevated 24 hour blood pressure results. She was allowed to move on to the renal function tests but had to reschedule a repeat 24 hour blood pressure monitor. The second 24 hour blood pressure results also returned elevated and she was referred to her cardiologist. Pending his review and finding, even though by this time she had passed the renal function tests, she was held from further candidate progress. Ultimately her blood pressure could be maintained within the standards expected for a kidney donor only with the use of two medications thus she was removed from the candidate pool. If you go back far enough all diseases have been rare at some time. The more common conditions like diseases of the kidneys didn’t become less rare because they affected more people. They became more common as those treating them spoke with others treating similar conditions comparing symptoms, patient histories, disease progression, and constants in presentation. Often when enough data is collected it becomes apparent the rare disease wasn’t as much rare as unrecognized. Treatment options and the responses then get shared, refined, retried, and publicized and the goal shifts from just education and proper diagnosis of the disease so difficult with the rare ones to effective treatment and some day eradication of the disease.
If you go back far enough all diseases have been rare at some time. The more common conditions like diseases of the kidneys didn’t become less rare because they affected more people. They became more common as those treating them spoke with others treating similar conditions comparing symptoms, patient histories, disease progression, and constants in presentation. Often when enough data is collected it becomes apparent the rare disease wasn’t as much rare as unrecognized. Treatment options and the responses then get shared, refined, retried, and publicized and the goal shifts from just education and proper diagnosis of the disease so difficult with the rare ones to effective treatment and some day eradication of the disease.
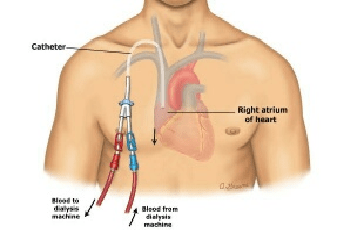 The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.
The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you. Again, thank you for staying on the journey with me. Coincidence continues. This month my transplant evaluation coincides with National Donate Life Month. Every April, Donate Life America celebrates National Donate Life Month, focusing national attention on every individual’s power to make life possible by registering as an organ, eye, and tissue donor, and learning more about living donation. Many years ago I registered to be a donor. That was long before I ever suspected I would someday be looking at transplants from a recipient’s perspective. If you’d like to explore becoming an organ or tissue donor, check with your local transplant center, your personal physician or the
Again, thank you for staying on the journey with me. Coincidence continues. This month my transplant evaluation coincides with National Donate Life Month. Every April, Donate Life America celebrates National Donate Life Month, focusing national attention on every individual’s power to make life possible by registering as an organ, eye, and tissue donor, and learning more about living donation. Many years ago I registered to be a donor. That was long before I ever suspected I would someday be looking at transplants from a recipient’s perspective. If you’d like to explore becoming an organ or tissue donor, check with your local transplant center, your personal physician or the