As I write this, a few minutes before 4:00pm on May 28, it is a year to the minute that I was getting home from what I hoped would be my last dialysis session. In 12 hours, I would be waking up for a ride to the hospital to have a kidney transplanted into me from my sister. For months after the evaluation process identified her as a candidate and a date was set, the staff at the dialysis clinic would say to me, “it won’t be long now,” or “are you counting the days yet,” or similar words of what they certainly thought were ones of encouragement. I met each one with “I’m not counting any chickens” That last day I think I said, “thanks, you’ve all been nice enough to me you but I hope I never see you again.”
We’ve now made it to a minute after 4:00pm on May 28 and it is juat about a year to the minute that the phone rang with a call from the transplant surgeon’s office. “Doctor wants you to come in this evening so she can run a new CT scan and do as much site review as possible before you get to surgery.” Because of previous abdominal surgeries my insides did not conform to the textbook illustrations budding surgeons poured over in their early med school days. They didn’t even conform to the messy real life version most people walk around with that present to surgeons many years past the book learning phase. Even though I had been scanned and rayed and imaged from every imaginable angle (and 1 of 2 unimaginable) I saw her point. I called my chauffeur who doubles as may daughter on her days off and asked one of them to take me to the hospital. But I still wasn’t going to start counting any chickens.
You’ve read the tale. The operation was a success but the implant didn’t take. Nineteen days later I was finally discharged with instructions to resume dialysis.
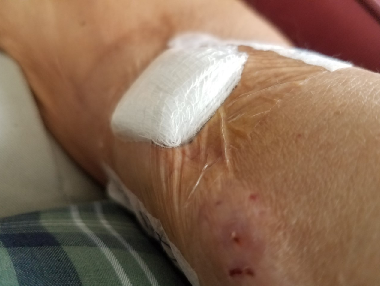
I never felt right at dialysis after that. Not mentally or emotionally not right but physically not right. In the best of times, and there are best of times in dialysis they just aren’t very good, one doesn’t feel right. It’s hard in the body and although it leaves you with sparkling clean blood (I used to refer to the dialysis unit as a bloodromat) it also leaves you with headaches, dizziness, tingking or numb extremities, a little bit of nausea, a lot of muscle cramps, and the need to sleep for 48 hours when you get to do it all over again. But this “not good” feeling was different. All of the above multiplied plus more and others and few etcetera.
Discussions with the doctor led to new and different tests which led to yet another tale. The transplant didn’t work but I was getting better in spite of it and became one of the few who have successfully been discharge from chronic dialysis.
So, now on the eve of what would be my first kidneyversary celebrating a new normal I am celebrating 4 months of being relatively normally normal.
I still have blood drawn every couple of weeks and see the doctor every couple of months. I still watch my diet, my fluid intake, and my other medications. I still pray every morning and every night. But I don’t still go to dialysis.
And I still don’t count chickens!
One other thing, my sister is still doing well also. Thanks Sis!






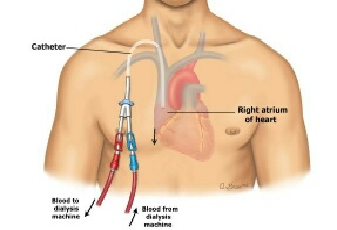 The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.
The unfortunate thing about dialysis catheters is that unlike say administration ports one might receive chemo through, they terminate outside the body and do so on a pair of tails. I’m posting a drawing so you can better see what I am trying to describe. (I could take a picture of my actual catheter but it’s not a selfie I’m anxious to snap and if you just type “dialysis catheter” into your favorite search engine you’ll get no end of new disgusting pictures to peruse at your leisure.) The part of the catheter inside floats and can actually be felt depending in where the tip resides at any particular moment. Reaching for anything higher than one’s shoulder, which given my modest height is anything off the counter, means moving the catheter around in there, also rather obviously noted. And because there is really no good way to anchor the outside tails, any movement or position change comes with a reminder that there is a part of you that isn’t really a part of you.